On July 26, Brooklyn announced results from the Phase II INSPIRE trial of IRX-2, a multi-cytokine biological immunotherapy. The trial was designed to evaluate the efficacy and safety of neoadjuvant therapy IRX-2 in combination with standard therapy in patients with newly diagnosed stage II, III or IVA oral squamous cell carcinoma. The data showed that the IRX-2 neoadjuvant group did not meet the primary endpoint. Brooklyn plans to present the results of the INSPIRE study at an academic conference in the second half of the year.
Oral squamous cell carcinoma (OCSCC) is one of the most common malignancies. There are approximately 34,000 OCSCC patients in the United States each year, and the cure rate is approximately 50%-60%. Patients in the early clinical stage are treated by surgery, combined with radiotherapy or chemotherapy, and the treatment effect is good, and the cure rate is high; while the patients in the middle and late clinical stage may have lymph node metastasis, the situation is relatively complicated, and the treatment effect is not good.
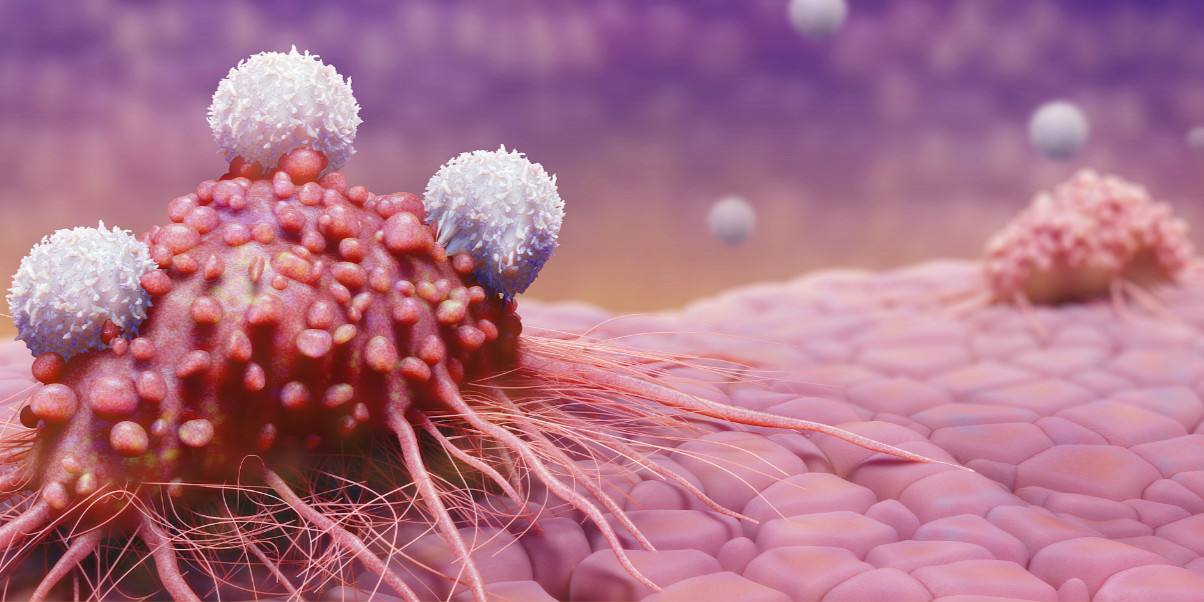
IRX-2 is an investigational primary cell-derived multi-cytokine bioimmunotherapy containing more than 29 cytokines designed to activate T cells to generate anti-tumor immune responses. IRX-2 is produced after stimulation of human peripheral blood mononuclear cells (PBMCs) by phytohemagglutinin (PHA). PBMCs are any peripheral blood cells with round nuclei, mainly composed of lymphocytes (T cells, B cells, NK cells) and monocytes. PHA-induced cytokine secretion mimics the process by which pathogens stimulate immune cell responses.
The INSPIRE study was a randomized, open-label trial of 150 patients with OCSCC. The experimental group received IRX-2+ standard treatment, and the control group received standard treatment. The primary endpoint was 2-year event-free survival (EFS), and secondary endpoints were overall survival (OS) and safety. Data showed that the median EFS in the intention-to-treat (ITT, n=105) population was 48.3 months (HR=1.10; 95% CI, 0.6-2.1, p=0.62), and the primary endpoint was not met.
Intent-to-treat analysis means that after patients complete randomization, for whatever reason they drop out of the trial or switch to another group, data analysis is still based on the original grouping. The aim was to reduce the effect of bias, since only analyzing so-called “complete data” would undermine the balance between groups.
Among key pre-specified subgroups by disease stage and type of adjuvant therapy, the IRX-2 arm had superior results. The IRX-2 group in the subgroup was less likely to experience an EFS event than the control group. The results of Kaplan-Meier analysis showed that in advanced (stage III and IV) patients, the 2-year EFS rate was 57.2 (40.3, 70.9) in the IRX-2 group and 49.4 (28.3, 67.4) in the control group; Among patients who received chemotherapy (radiotherapy only) as part of adjuvant therapy, the 2-year EFS rate was 76.4 (52.2, 89.4) in the IRX-2 group and 60.6 (29.4, 81.4) in the control group. However, the rate of adverse events related to study treatment was higher in the IRX-2 group than in the control group (55.9% vs 40%), mainly due to injection site reactions and fatigue.
“We thank the patients and their families for participating in this trial,” said Roger Sidhu, MD, Brooklyn’s chief medical officer. “IRX-2 immunotherapy, administered as a local subcutaneous injection, was well tolerated in the oral squamous cell head and neck cancer patient population. We noted a trend toward better EFS for IRX-2 in advanced patients and in patients who did not receive chemotherapy as part of adjuvant therapy. These patients represent a large proportion of patients with head and neck cancer and represent a patient population with a high unmet clinical need The mechanism of action of IRX-2 and preclinical and translational medicine studies have demonstrated its potential synergy with immune checkpoint inhibitors as a novel combination immunotherapy strategy for potentially ineligible or in need of intensive adjuvant adjuvant be explored in treated patients.”
“The INSPIRE study achieved its primary goal of identifying a patient population that may benefit from IRX-2 as neoadjuvant therapy,” said Dr. Matt Angel, CEO of Brooklyn. “These encouraging results justify the design of the INSPIRE study and add to the Provides a clear way forward for evaluation in patient populations who may benefit from IRX-2 in combination with checkpoint inhibitors. The ability to provide an effective and well-tolerated treatment for patients with advanced head and neck cancer who cannot receive chemotherapy is very exciting. People are excited.”