Given the complex roles of macrophages, both good and evil, in various biological contexts, researchers have been exploring their abundance and function. This guide outlines the genes expressed by macrophages and the immunological tools available for detection.
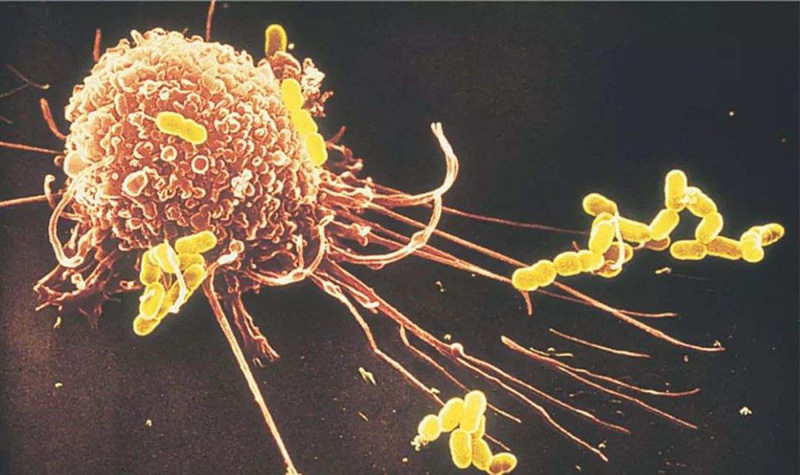
Macrophages are widely distributed white blood cells that exist in various tissues of the human body. As part of the mononuclear phagocyte system, macrophages function to engulf dead cells, cellular debris, pathogens, and other foreign substances. In addition, they have signaling and regulatory functions and are involved in many biological processes, such as immunity, development, repair, homeostasis, and cancer.
Given the complex roles of macrophages, both good and evil, in various biological contexts, researchers have been exploring their abundance and function. This guide outlines the genes expressed by macrophages and the immunological tools available for detection. Targeting these proteins not only identifies subtypes of macrophages, but also aids in the study of associated pathways or disease states.
In addition to playing specific roles in various tissues, macrophages are highly plastic and can change their phenotype in response to environmental cues. This allows macrophages to form distinct subpopulations, each with distinct gene expression profiles and cellular functions. To better understand these differences, we classify various protein markers here.
Markers in monocyte-macrophage transformation
The source of macrophages is a complex issue. Mouse studies have shown that macrophages are derived either from embryonic precursor cells or from bone marrow-derived monocytes. Monocytes circulating in the blood migrate to tissues to form tissue-resident macrophages (TRMs). This closely related cell type efficiently replenishes macrophages in tissues. To differentiate macrophages from their precursors, one typically detects a panel of cell surface markers and their differential expression levels.
Antibodies to detect monocyte lineage markers include: Ly6c1 antibody, F4/80 antibody, ITGAM/CD11b antibody, CD68 antibody, FCGR3A/CD16 antibody, CD14 antibody
Markers of tissue-resident macrophages
Macrophages reside in different tissues, giving rise to populations of cells that perform different functions. Studies in mice have shown that macrophage phenotype and function are determined by the signals they receive in the tissue microenvironment. In addition to being the first line of defense against pathogen invasion, resident macrophages also play an important role in maintaining tissue integrity and tissue homeostasis.
For example, macrophages (microglia) that develop in the central nervous system have been found to perform a variety of functions, including scavenging debris, remodeling synaptic connections, and immune surveillance. In adipose tissue, adipose-associated macrophages are involved in signaling that regulates insulin sensitivity. Alveolar macrophages attack inhaled foreign bodies and remove excess pulmonary surfactant by phagocytosis. Macrophages in the liver, known as Kupffer cells, clear the blood of microorganisms, red blood cells, and other cellular debris. Bone marrow macrophages can promote the hematopoiesis of red blood cells. Macrophages in the spleen are involved in activities such as immune surveillance, iron metabolism, and cellular clearance.
Markers of M1 and M2 polarization
Under appropriate stimulation, macrophages are activated into different inflammatory states, including M1 (classical activation) and M2 (selective activation). M1 macrophages are pro-inflammatory and are associated with immune responses to bacterial and intracellular pathogens. In contrast, M2 is anti-inflammatory and functions in angiogenesis and wound healing. M2 is also associated with T helper 2 (Th2) responses, such as antihelminth immunity, asthma and allergies.
Activation of M1-type macrophages occurs through signaling through IFNG, TNF, and Toll-like receptors (TLRs). Genetic markers associated with M1 polarization include IL1a, IL1b, IL6, NOS2, TLR2, TLR4, CD80 and CD86. For M2 macrophages, activation is through cytokines such as IL4, IL10, and IL13. M2 markers include CD115, CD206, PPARG, ARG1, CD163, CD301, Dectin-1, PDL2 and Fizz1. Notably, the M1 and M2 phenotypes are contiguous, so macrophages in the middle range can express some markers simultaneously.
Antibodies for detecting M1 markers include: IL1B antibody, NOS2 antibody, TLR2 antibody, CD86 antibody; antibodies for detecting M2 markers include: CSF1R/CD115 antibody, MRC1/CD206 antibody, ARG1 antibody, CD163 antibody
Markers of tumor-associated macrophages
It has been found that cancer cells can also use macrophages to promote cancer development. For many types of cancer, increased density of macrophages at tumor sites is associated with poor patient survival. Mouse studies have also found that tumor-associated macrophages (TAMs) can stimulate tumor angiogenesis, assist tumor cell migration and invasion, and suppress tumor immunity.
These results can be attributed to cancer cell signaling affecting macrophage function, and proteins produced by TAMs themselves that promote tumor growth. Cancer biology is inherently complex, and likewise, TAMs can employ different gene expression profiles. Some of the TAM markers mentioned in the literature include CCR2, CSF1R, MARCO, PDL2, CD40, CCL2, CSF1, CD16 and PDGF beta. The interrelationship between macrophages remains an active area in cancer research and drug development.
Antibodies to detect TAM markers: CCR2 antibody, PDL2 antibody, CD40 antibody, CCL2 antibody, PDGFB antibody.