Since the launch of the first CAR-T cell therapy in 2017, the era of cell therapy has officially begun, and good clinical results have been achieved in the treatment of various tumors, and the number of available targets is also rapidly increasing. The success of CAR-T in the field of tumor treatment has fueled scientific and clinical interest in using CAR-T as a treatment for other types of diseases. They are trying to explore the future development trend of CAR-T cell therapy from different perspectives.
Recently, Biomedicines published a review entitled “Application of CAR-T Cell Therapy beyond Oncology: Autoimmune Diseases and Viral Infections”. In this review, researchers focus on diseases beyond the field of oncology by focusing on CAR-T. , such as autoimmune diseases and viral infections, including SARS-CoV-2, provides an overview of modern trends and recent developments in CAR-T cell therapy from a fresh perspective.
The full name of CAR-T cell therapy is Chimeric antigen receotor T cell therapy, that is, chimeric antigen receptor T cell therapy. The principle is to collect the patient’s own T cells, transform them in vitro through genetic technology, load them with receptors and costimulatory molecules that recognize tumor antigens, and at the same time, expand them in vitro and then infuse them back into the patient’s body to make them. It can effectively identify and kill tumor cells more accurately.
Despite different etiologies, the pathogenesis of some diseases may have similarities with tumors, and these commonalities may enable them to be treated by CAR-T therapy. In addition, in many cases, the human immune system will be partially dysfunctional due to the occurrence of diseases, and CAR-T can serve as a powerful substitute for the human immune system and play a certain protective role in the human body.
CAR-T cells and autoimmune diseases
The pathogenesis of many autoimmune diseases (AIDs) has not yet been determined, but it is certain that T cell tolerance failure plays an important role in the pathogenesis of these diseases. Potential mechanisms of loss of immune self-tolerance in AID include activation of autoreactive B cells, which produce autoantibodies that promote tissue damage, and inhibition of cytotoxic or regulatory T cells.
Chimeric autoantibody receptor (CARR) T cells target autoantibody proteins on the surface of autoreactive B cells, and only have selective cytotoxicity against immune cells carrying specific autoantibodies without causing immunosuppression. Thus, such cells can directly eliminate surface immunoglobulin memory B cells and indirectly eliminate transient plasma cells that produce pathogenic autoantibodies. In addition, since regulatory T cells (Tregs) in autoimmune diseases are often suppressed in AID, researchers formed CAR-Tregs by transducing FOXP3 into T cells to modulate the function and viability of Tregs in patients.
There have been studies using CARR-T cells to treat Pemphigus vulgaris (PV), an autoimmune disease caused by autoantibodies against the keratinocyte adhesion protein Dsg3. The researchers used the principle of CARR-T cells to design Dsg3-CARRT cells and enter them into a PV mouse model, and observed that the cell therapy showed specific elimination of anti-Dsg3 B cells in the PV mouse model, while no any adverse reactions.
In addition, CAR-T cell therapy has also been used to study the treatment of autoimmune diseases such as hemophilia, type 1 diabetes, multiple sclerosis, systemic myasthenia gravis, systemic lupus erythematosus, and neuromyelitis optica spectrum disorder. middle.
CAR-T cell therapy and infectious diseases
Chronic hepatitis B virus (HBV) patients usually have low immunity, and long-term development is likely to lead to the occurrence of liver cancer. Based on CAR-T cell therapy, researchers designed a CAR-T cell that can specifically recognize hepatitis B virus surface antigen (HBsAg), and evaluated its ability to recognize HBV+ cells and HBsAg particles in vitro. Its efficacy on HBV-infected hepatocytes was tested in a human liver chimeric mouse model. The results showed that anti-HBsAg-CAR T cells could recognize HBsAg particles and HBV+ cells in vitro, and could effectively reduce HBV-DNA and HBsAg levels in mice.
Chronic hepatitis C virus (HCV) infection is a medical indication for liver transplantation in patients with end-stage chronic infection who do not respond to current treatments. For many HCV patients, the risk of reinfection after treatment remains high, which means that effective alternative therapies need to be developed. To this end, the researchers designed CAR-T cells that recognize the HCV E2 glycoprotein, a major target of the host immune response, and the results showed that anti-HCV/E2 CAR-T cells exhibited significant cytotoxicity against HCV-infected cells.
In addition, many more researchers are trying to explore the role of CAR-T cell therapy in other viral infectious diseases. For example, human cytomegalovirus infection and influenza A virus infection. The above studies provide the basis for further exploration of CAR-T cell therapy in the treatment of various infectious diseases.
CAR-T cell therapy and other intractable diseases
AIDS is an acquired immunodeficiency syndrome caused by human immunodeficiency virus. Up to now, AIDS is still a worldwide medical problem. Once infected with the virus, there is no cure, and the occurrence and development of the disease can only be controlled through antiviral therapy.
Since the cytotoxicity of CD8+ T cells to HIV-1 plays a key role in the control of HIV-1 infection, it also provides an effective way to use CAR-T cell therapy for HIV-1 treatment. The therapeutic target of anti-HIV-1 CAR-T cells is the gp120 region of the HIV envelope glycoprotein expressed on the surface of HIV-infected cells. The researchers designed CD4+ CAR-T cells, and after in vitro tests, the researchers found that CD4+ CAR-T cells could effectively inhibit the replication of HIV virus while destroying HIV virus-infected T cells. In addition, the researchers found that patients treated with CAR-T cell therapy had lower rates of viral rebound and significant reductions in intestinal HIV DNA, suggesting that CD4+ CAR-T cells can indeed influence tissue viral reservoirs.
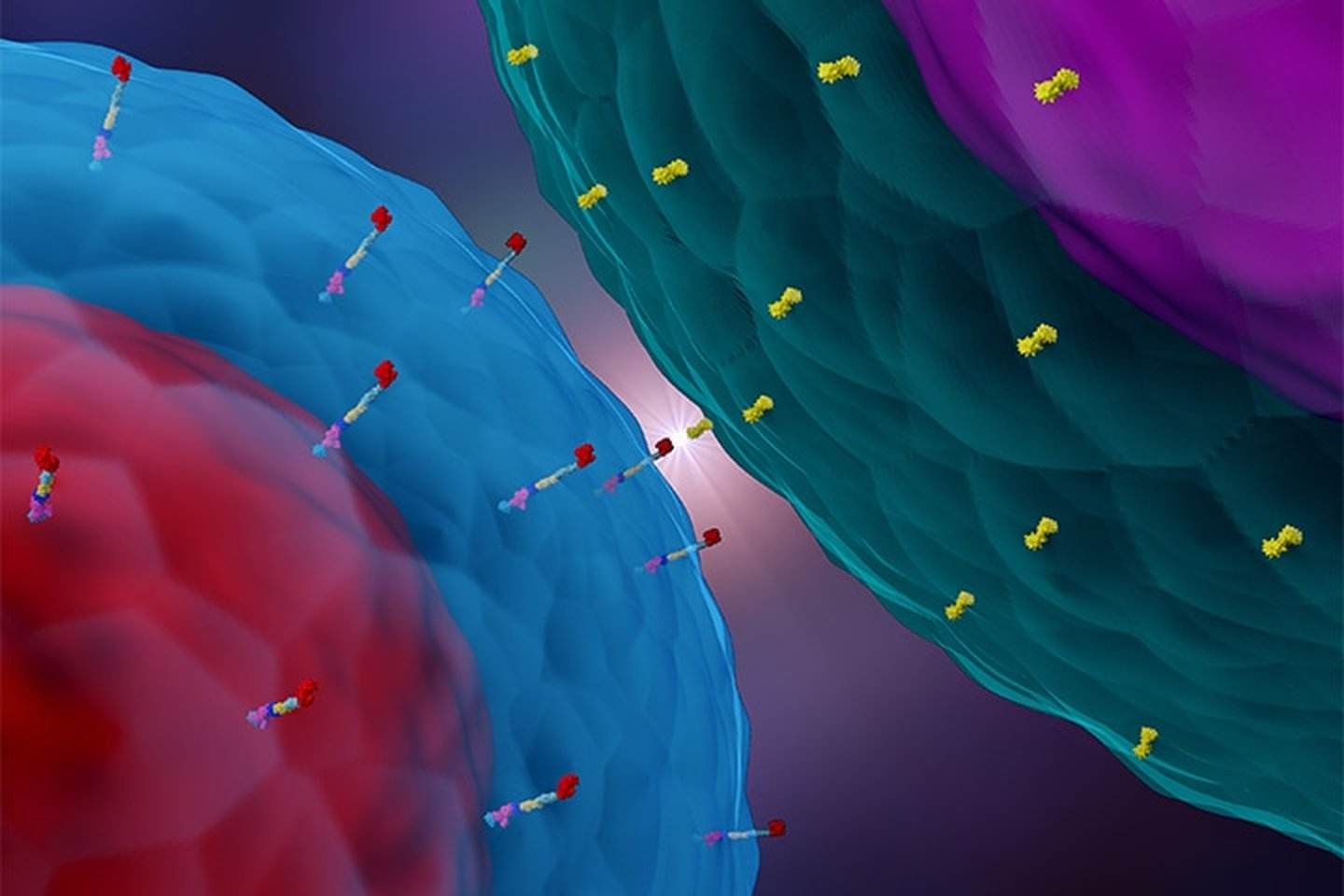
In addition to AIDS, CAR-T cell therapy has also been used in the treatment of COVID-19. The researchers attempted to develop CAR-NK cells to target the SARS-CoV-2 spike protein with the CR3022 scFv domain, and through in vitro experiments, they found that CR3022 CAR-NK cells were able to eliminate SARS-CoV-2-infected cells. In addition to this, clinical trials evaluating bispecific NKG2D-ACE2 CAR-NK cell therapy (Figure 4) are also underway.
It can be seen from the above studies that with the continuous development of the understanding and understanding of various pathologies and their molecular mechanisms, the medical application of CAR-T cell immunotherapy will go far beyond the field of tumor. An increasing number of molecules have been demonstrated as therapeutic targets for a variety of diseases, making CAR-T cell therapy an attractive and promising treatment option.
From tumors to autoimmune diseases to various infectious diseases, the application scope of CAR-T cell therapy is constantly expanding. It is believed that with the continuous increase of disease targets and the continuous upgrading of CAR-T cell technology, the future may There are more refractory diseases that can be treated by CAR-T cell therapy, achieving all diseases and CAR-T.